The Apc Payment System Is Based On What Coding System?
The apc payment system is based on what coding system?. APCs are similar to DRGs. The APC is the service classification system for the outpatient prospective payment system. CPTHCPCS codes Question 10 0 out of 1 points The Accounts Receivable Department as the hospital needs to know how much Medicare paid on claims so they can drop the balance to secondary insurance.
Under the OPPS on which code set is the APC system primarily based for outpatient procedures and services including devices. Therefore the APC payment rate for APCs 5853 and 5863 is based on a per diem amount. CPT and HCPCS After the assignment of appropriate diagnostic and procedure codes have been assigned to a record what is the next step to complete for a provider to be reimbursed under a.
APCs or Ambulatory Payment Classifications are the governments method of paying facilities for outpatient services for the Medicare program. Out of 1 points The APC payment system is based on what coding system Selected from HIM 2956 at Rasmussen College. TCO 5 The APC payment system is based on what coding system Student Answer from HIM 3750 at Western Governors University.
CPTHCPCS codes The comprehensive assessment tool that captures data for the. Medicare adjusts outpatient prospective payment system payment rates for 11 cancer centers so that the payment-to-cost ratio PCR for each cancer center is equal to the average PCR for all hospitals. - Basic unit of the ambulatory payment classification system APC system.
Click to see full answer. APCs or Ambulatory Payment Classifications are the United States governments method of paying for facility outpatient services for the Medicare United States program. CPTHCPCS codes ICD-9-CM diagnosis and procedure codes CPT and ICD-9-CM procedure codes Only CPT codes.
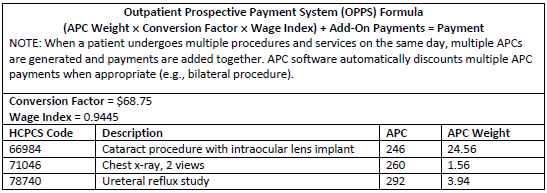
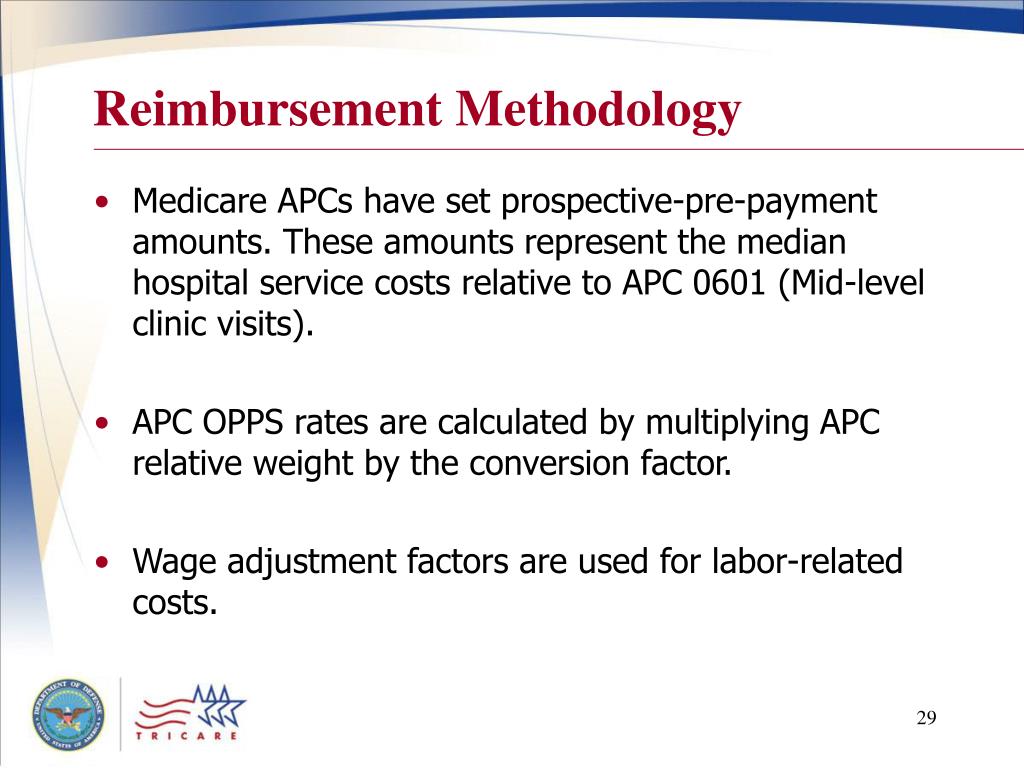
CMS assigns to facilitate billing and payment through a New Technology APC is independent of the other two coding systems and intended solely for hospitals to. Within a group the diagnnoses and procedures are similar in terms of resources used complexity of illness and conditions represented. The payments for APCs are calculated by multiplying the APCs relative weight by the OPPS conversion factor with a slight adjustment based on the geographic location.
Identify procedures and services that cannot be billed together on the same day of service for a patient. Promoting correct coding and control of inappropriate payments is the basis of NCCI claims processing edits that help identify claims not meeting medical necessity.
APCs or Ambulatory Payment Classifications are the United States governments method of paying for facility outpatient services for the Medicare United States program.
- Basic unit of the ambulatory payment classification system APC system. A single payment is made for the outpatient services provided. The APC for each procedure or service is associated with an OPPS SI which. Ambulatory payment classifications APCs are based on ICD-9-CM codes. CPTHCPCS codes Question 10 0 out of 1 points The Accounts Receivable Department as the hospital needs to know how much Medicare paid on claims so they can drop the balance to secondary insurance. Within a group the diagnnoses and procedures are similar in terms of resources used complexity of illness and conditions represented. Therefore the APC payment rate for APCs 5853 and 5863 is based on a per diem amount. Ambulatory payment classifications APCs are a classification system for outpatient services. The APC payment system is based on what coding system.
Both APCs and DRGs cover only the hospital fees and not the professional fees associated with a hospital outpatient visit or inpatient stay. The payments for APCs are calculated by multiplying the APCs relative weight by the OPPS conversion factor with a slight adjustment based on the geographic location. CPTHCPCS codes ICD-9-CM diagnosis and procedure codes CPT and ICD-9-CM procedure codes Only CPT codes. APCs or Ambulatory Payment Classifications are the United States governments method of paying for facility outpatient services for the Medicare United States program. Ambulatory payment classifications APCs are based on ICD-9-CM codes. One major difference between the DRG and APC systems is that an inpatient may be assigned more than one DRG code per hospital admission whereas an outpatient is assigned only one APC code per hospital encounter. Medicare adjusts outpatient prospective payment system payment rates for 11 cancer centers so that the payment-to-cost ratio PCR for each cancer center is equal to the average PCR for all hospitals.























Posting Komentar untuk "The Apc Payment System Is Based On What Coding System?"